While breathing a certain way may seem simplistic, and perhaps even irrelevant to conditions such as pelvic organ prolapse, it is in fact true that natural breathing while under the forces of gravity is what creates and maintains the pelvic organ support system.
Conventional culture teaches that the rib cage should expand out to the sides with each in-breath. However, the lower ribs can only expand laterally when the upper abdominal wall is held in. Western women like the look of a small waist, so they cultivate a small midriff by habitually holding in their upper abdominal wall. It is not surprising therefore, that the type of breathing that supports a small waist is generally considered ‘natural’ by yoga and physical therapy. Reversal of natural breathing is the single most important factor in loss of pelvic organ support.

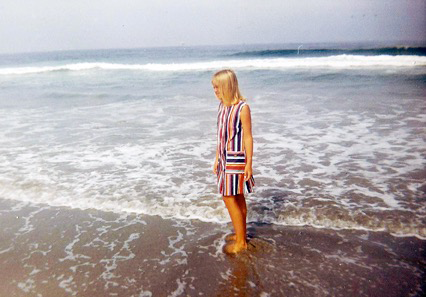
All healthy babies and young children breathe naturally. The...